Abstract
Background Multiple cancer registries including SEER and NCDB have repeatedly demonstrated increased mortality in non-white AML patients, with the survival disparity widening over the past 2 decades. A recent mediation analysis conducted in our newly created Chicago AML registry suggests that the Black-White and Hispanic-White survival disparity is significantly mediated by census tract variables (tract affluence, disadvantage and segregation) and these serve as surrogates for structural racism (Abraham et al. Blood 2022).
In the current study we try to operationalize the mechanisms of structural racism contributing to disparities in myeloid malignancies
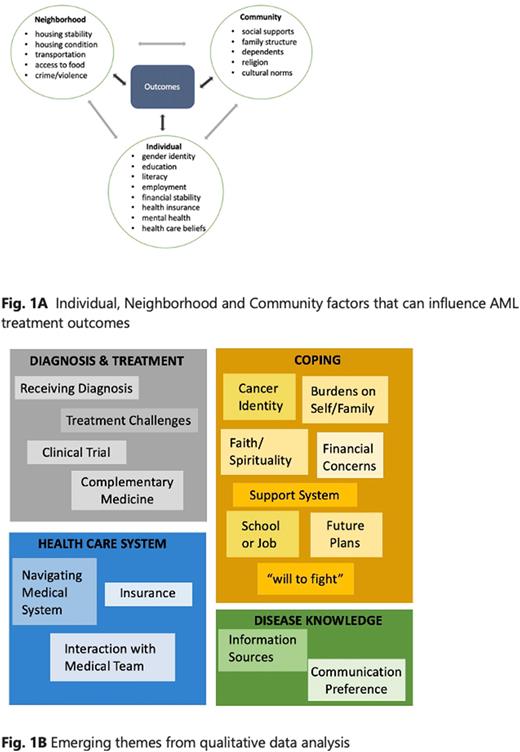
Methods A prospective mixed-methods approach using quantitative (questionnaires) and qualitative (semi-structured interviews) methods is employed to uncover the complex interrelationship between individual, neighborhood/built environment and community level factors (Fig. 1A) that can influence treatment outcomes. Patients are enrolled 30-90 days from diagnosis and will be followed for two years. Validated questionnaires evaluate: patients' neighborhood and environmental living conditions (AHC HRSN), health literacy (CHLT-6), financial toxicity (COST-FACIT), medication affordability/adherence (ARMS), and mental health (PHQ-4). This is complemented by qualitative data from semi-structured interviews. The transcripts are processed and coded, using a qualitative data management software, and emerging themes noted (Fig. 1B).
Results Data collection is ongoing and completed on 18 patients with aggressive hematologic malignancies, majority with AML and high risk MDS. The median age is 56 years with 50% self-declaring as NHW, the remainder NHB, Hispanic and Asian. Only 25% received a college education, 50% reported a median household income below $50,000, and the patient was the primary or sole financial provider for the family in one-half of cases. While most patients did not report struggles with insurance coverage and out of pocket costs on the questionnaire, they did express worry about long-term consequences such as job security and financial well-being. Financial toxicity was highest and health literacy lowest in the NHB patients.
62% reported access to internet and 50% had smartphones. Patients did not endorse concerns about housing or neighborhood conditions influencing their health care. Medication affordability/adherence was adequate across groups. Most patients felt sufficiently supported by family for transportation but 25% reported that they could use more help with ADLs.
One-half of patients reported feeling loneliness and stress on the PHQ-4 questionnaire, and detailed the consequences of a long hospitalization (isolation, missing family events) in interviews. Adolescent and young adult (AYA) patients also discussed grappling with their newfound cancer identity. Notably, 25% of patients reported >5 alcoholic drinks /day for men or >4/day for women. Medical mistrust was not reported, most patients expressed trust/confidence in their treatment team which was improved by regular communication and responsiveness.
Discussion The mixed methods approach offers an ample source of data from both questionnaires and interviews for a fuller understanding of factors that can influence inequity in the delivery of leukemia care.
The unique perspectives of an understudied population at a minority serving cancer identified targetable barriers to care. There is broad need for additional assistance at home for ADLs, mental health concerns as well as significant levels of alcohol use which have not been previously explored. A third of patients lacked access to regular internet, an important source of education and communication that could widen health inequities.
Patients expressed unique challenges specific to AML including the prolonged hospitalizations resulting isolation, and difficulty coping with the cancer identity reported by the AYA population. Regular communication with a responsive medical team contributed positively to patient-provider relationships.
Ongoing work includes i) expanding the current cohort across a broader socioeconomic spectrum to further enrich the data ii) prospectively linking this data to treatment complications and outcomes. The results of this study can guide future strategies for targeting resources and interventions to narrow leukemia outcome disparities.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal